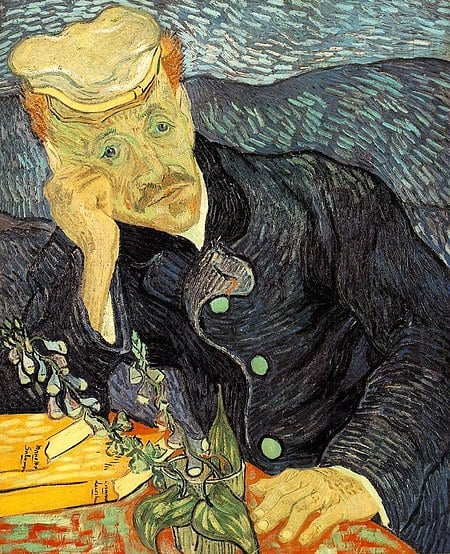
Physician burnout—Part 1
In our department at UMass Chan Medical School, the Department of Family Medicine and Community Health, we have a listserv. Yes, that software relic of the digital past that is nevertheless used extensively in healthcare because listserv technology, while simple, is relatively secure. Not many clinicians post things on our listserv, but when they do, the posts can kick off lengthy debates about the topic in question. It is good to have practitioners sharing their views in a safe space.
Recently, one of our family doctors posted a link to an article in the New England Journal of Medicine [the article can be found here] about physician burnout, recently a hot topic purporting epidemic levels of physician burnout with not only personal impact but also patient care implications. A nerve was touched. Drs. Wright and Katz, authors of the article, described a program in Colorado (APEX) that tackled burnout with a team-based approach to primary care practice. In our CIPC online course “Primary Care Behavioral Health” we also discuss the concept of supporting team members to work at the limit of their licenses. The roles of MAs, RNs, BHCs can be expanded to relieve the incredible administrative, documentation and regulatory burdens felt by PCPs and having a team allows the patient to interact with the best person to address the current need, rather than having only the physician address all of the patient’s needs. Often the physician is not the best (and certainly not the most economical) person to address the patient’s needs.
Creating an environment in which teams support PCPs also requires the PCP to give up some control. Traditionally, the physician “drives the bus”, which was fine before the regulatory and documentation demands became so daunting and the expectations for primary care increased in breadth and complexity. The NEJM article likens it to “texting while driving”. Wright and Katz cite time-motion studies that show, “for every hour physicians spend with patients, they spend one to two more hours finishing notes, documenting phone calls, ordering tests, reviewing results, responding to patient requests, prescribing medications, and communicating with staff.”
The APEX program the authors highlight required more than doubling the number of medical assistants and added many hours of in-depth training to allow them to “…gather data, reconcile medications, set the agenda for patient visits, and identify opportunities to increase preventive care.” They also act as scribes and provide patient education and health coaching. The results reported are impressive: Within 6 months after the APEX launch, burnout rates among clinicians dropped from 53% to 13%.
Recruiting and hiring replacement physicians is incredibly expensive, with most estimates far exceeding $250,000 per position. The benefits in the APEX case outweigh the costs. When our department introduced medical scribes, we found that it allowed physicians to see two more patients in the day, rendering the scribes cost neutral. One of our physicians commented, “That service makes a tremendous difference – enhancing interaction with the patient rather than inhibiting it.” The conversation around physician burnout has quickly become a conversation about improving practice efficiency and new models of primary care practice – not only for the undeniable benefit of the patient but now for the clinicians as well.