
→ James Andersen, PhD is the guest author of this blog post, outlining a collaboration on MAT between UMass CIPC and Bassett Health Systems.
→ "There are an estimated 91 Americans dying each day from heroin and opioid abuse..."
Opioid addiction: A national epidemic
Effective treatment options exist but are challenging to access, especially for patients who live in remote, rural areas. There is a long history of separation of treatment of addiction and medicine and a disconnect between primary care and treatment for opioid addiction. Our project has brought evidence-based treatment to a population in great need. We have treated nearly 200 patients with buprenorphine for opioid addiction. We have 27 primary care clinicians who have obtained their Drug Addiction Treatment Act (DATA) waivers. These waivers allow primary care clinicians to prescribe buprenorphine for treatment of opioid addiction.
is a well-supported approach to treatment, and previous research has demonstrated that this treatment can be effectively and safely delivered from a primary care setting (Ducharme, Fraser, & Gill, 2012; Bhatraju et al 2017). However, many patients do not access treatment. A 2016 US Surgeon General report estimated that only about 10% of people with addiction receive professional treatment. This project successfully built onto existing infrastructure (i.e., primary care clinics) to make evidence-based treatment more accessible to patients who have historically been underserved.
Collaboration with UMass Chan Medical School CIPC
Supported by Delivery System Reform Incentive Payment (DSRIP) funding, we have been fortunate to collaborate with the University of Massachusetts (UMass) to get primary care clinicians waivered, and confident and competent in using their waivers. We have met weekly with UMass for the last year via video conference, using the ECHO (Extension of Community Healthcare Outcomes) model. This innovative video conferencing hub-and-spoke model allows specialty knowledge to spread from an expert team (hub) to community primary care clinics (spokes), and for primary care teams to share practical, primary care focused expertise.
We have hired an addiction medicine psychiatrist who has been essential to our program, providing expert care and consultation to support our primary care clinicians. DSRIP has facilitated collaboration with Community-Based providers for wrap-around services as part of the model. The state has cited our project as one of the five best overall DSRIP projects in New York.
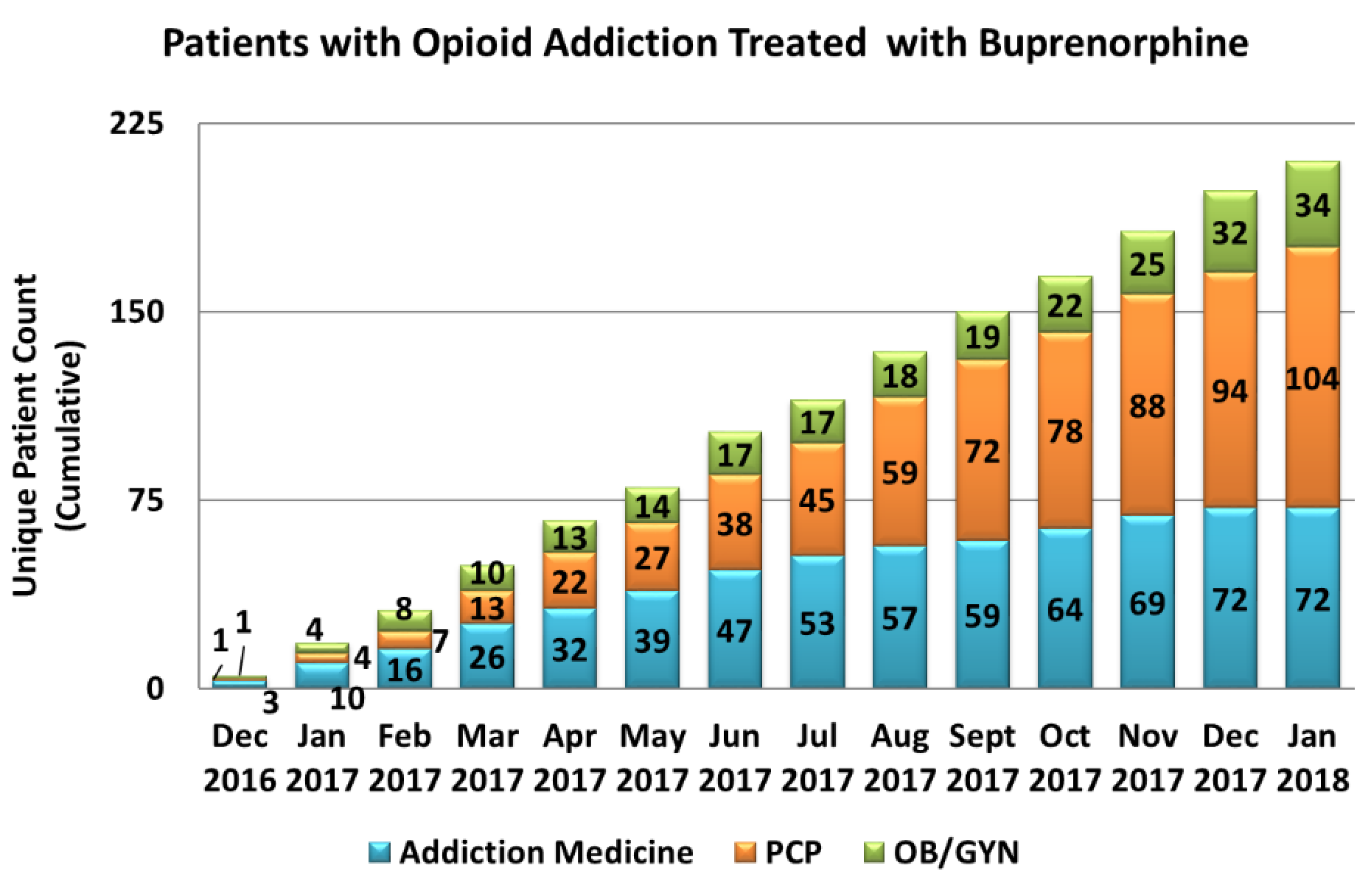
The chart below depicts the cumulative number of patients treated for Opioid Use Disorder (OUD) with buprenorphine within our network. The graph depicts unique patients who have received at least one buprenorphine prescription from a prescriber in our network. The provider group (i.e., PCP, Addiction Medicine, or OB/GYN) to whom the patient is attributed is based on who wrote the first prescription for the patient. From Dec 2016 through Mid Jan 2018, we have initiated treatment for 210 total patients in our network. 176 (84%) of those patients were treated by either addiction medicine and/or primary care. The remaining 34 patients (16%) were treated by OB/GYN physicians as part of their perinatal care.
Our OB/GYN department has been offering buprenorphine for OUD as part of the care they offer to pregnant patients since before we initiated our project, and the patients for whom they initiated treatment cannot be attributed to this project. However, because they are doing this important work makes it all the more important to have an infrastructure for ongoing maintenance treatment, as our obstetrician group does not continue to oversee care for patients with OUD after they have given birth.
Why the use of primary care clinics
There are many reasons that we chose to use primary care clinics to house this effort, including the capacity to identify and manage co-morbid medical conditions (pregnancy, HIV, Hepatitis C, etc) that relate to opioid addiction, accessibility for a rural community, and the ability to sustain gains into the future. One resource that we know will be around for patients long-term is primary care. By weaving this treatment into primary care services and conceptualizing it as management of a chronic health condition (similar to diabetes or hypertension), it fits within the purview of whole-person primary care to which primary care clinicians are accustomed.
Moreover, building the service into primary care helps make it accessible to more patients regardless of income, as primary care visits within our network are covered by both private insurance and Medicaid. We currently have five clinics serving patients across four counties who have joined this effort and plan to add more over this next year. We are aiming to have at least 90% of our network’s primary care clinics offering this as part of comprehensive primary care within the next three years.
"...there are an estimated 91 Americans dying each day from heroin and opioid abuse..."
We believe that this effort is replicable by other networks across the state and the nation. Any primary care clinician can obtain his or her “X” license. The course takes eight hours for physicians and 20 hours for Advanced Practice Clinicians (APCs: nurse practitioners and physician assistants). One of the main reasons that we chose to use primary care as the home for this work is an appreciation for the need to match treatment availability to patient need. Primary care is available in most communities around the state. Were buprenorphine management for opioid addiction to become part of the standard of primary care, it would certainly help bring treatment to scale. Though there are an estimated 91 Americans dying each day from heroin and opioid abuse, only one in ten people struggling with addiction ever gets professional treatment.
Get the latest updates on behavioral health and primary care
Subscribe
About the Author:

Dr. Andersen is a former behavioral health fellow at UMass Chan Medical School Department of Family Medicine and Community Health and is currently Leatherstocking Collaborative Health Partners DSRIP Medical Director