News from the UMass Diabetes Center of Excellence
-
Tuesday, February 03, 2026
![Dr. Louis Messina, MD Wound Healing Study]()
-
Friday, January 23, 2026
![SCDC Co-Directors]()
-
Thursday, December 04, 2025
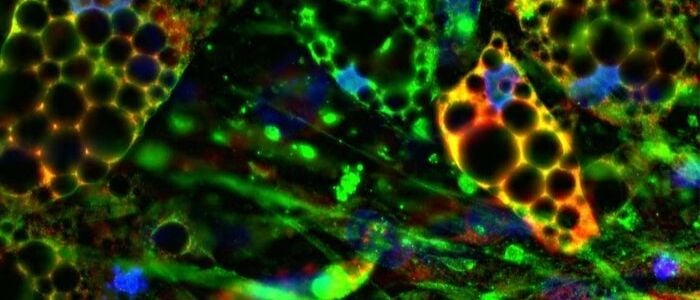
![Silvia Corvera lab fat cells image]()
-
Wednesday, November 19, 2025
![Diabetic Foot Clinic 2024]()
-
Friday, October 17, 2025
![Liver Research at UMass Chan Medical School]()
-
Friday, September 26, 2025
![Nuzzy Memorial Golf Tournament]()
-
Friday, August 01, 2025
![UMass Diabetes Humanized Mouse Core Dale Greiner and Michael Brehm]()
-
Thursday, July 24, 2025
![Cytokine-Stressed Human Pancreatic Islets]()
-
Friday, September 05, 2025
![Virtual Diabetes Camp]()
-
Friday, June 20, 2025
![Diabetes Management Technology Update]()
-
Monday, March 10, 2025
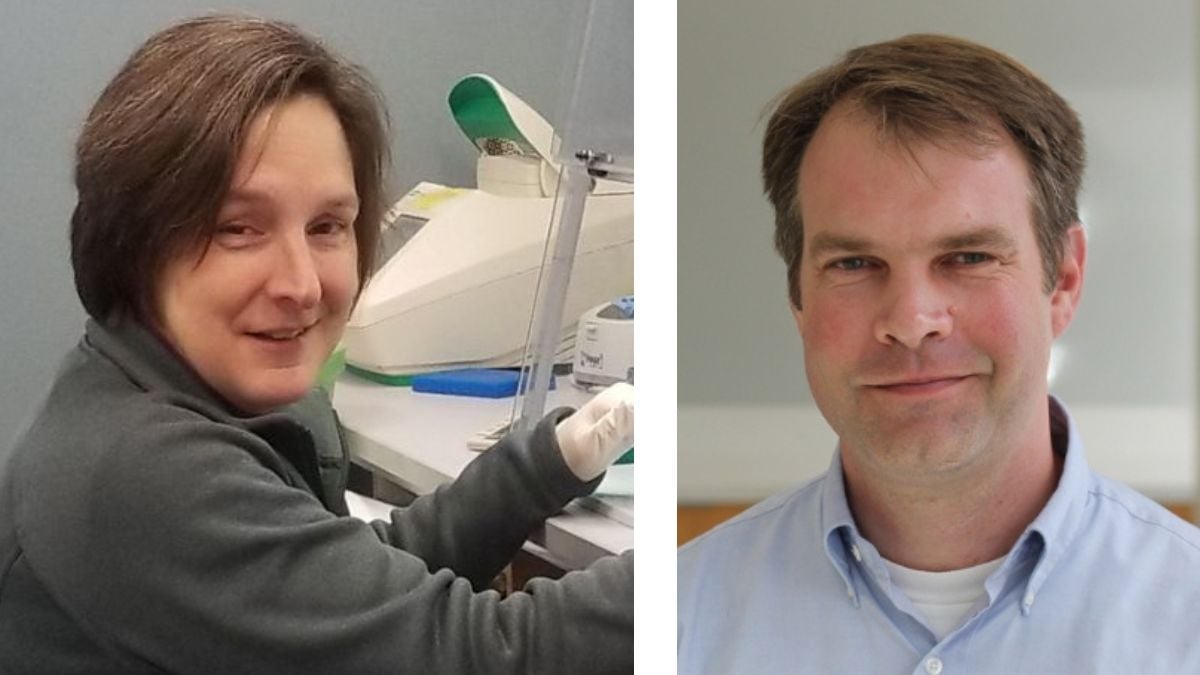
![Jessica Spinelli, PhD and graduate student Nicolai Hathiramani]()
-
Friday, January 24, 2025
-
Tuesday, May 20, 2025
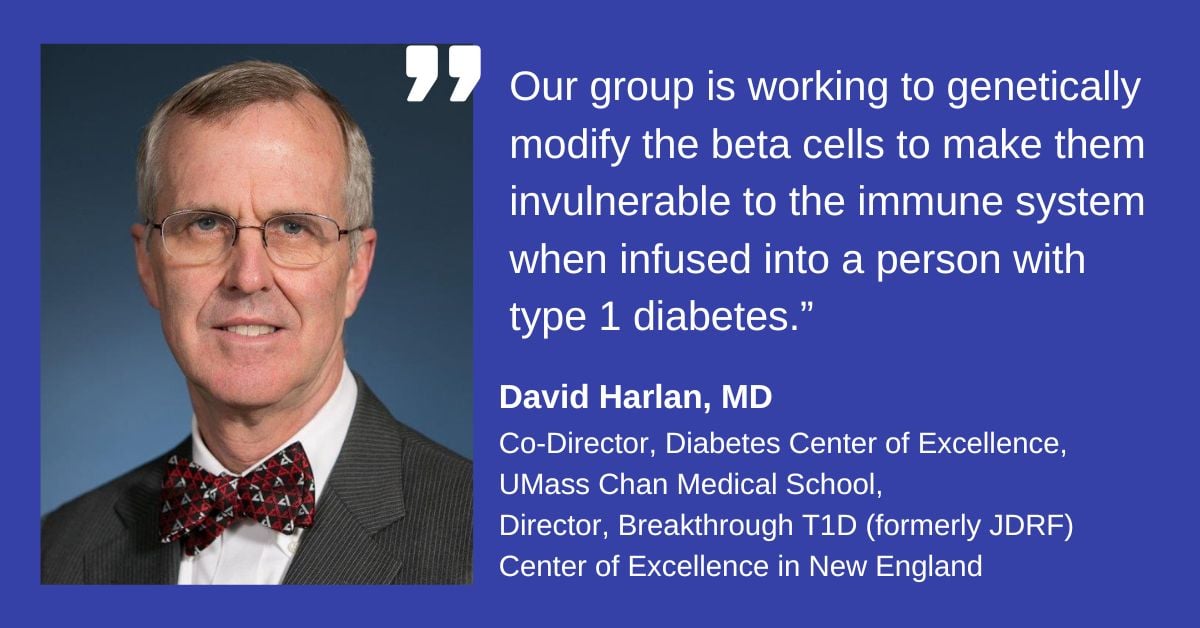
![Dr. David Harlan, MD, Breakthrough T1D Center of Excellence in New England Director]()
-
Wednesday, October 23, 2024
-
Friday, October 11, 2024
![Glucose Management in Pregnancy]()
-
Wednesday, October 09, 2024
![Adipocyte cell image]()
-
Tuesday, August 20, 2024
![Lou Messina Type 2 diabetes research UMass Chan Medical School]()
-
Friday, August 16, 2024
![Nate Farrington Diabetes Rainbow Report]()
-
Tuesday, July 23, 2024
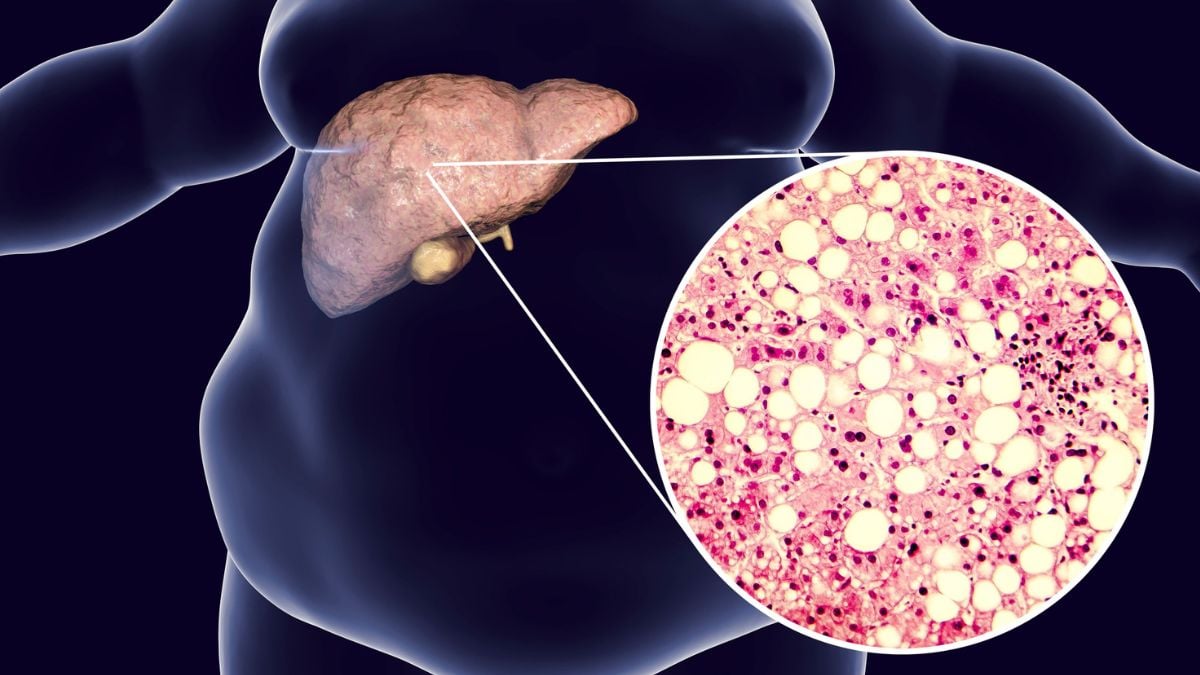
![Fatty Liver Disease and Diabetes]()
-
Friday, July 19, 2024
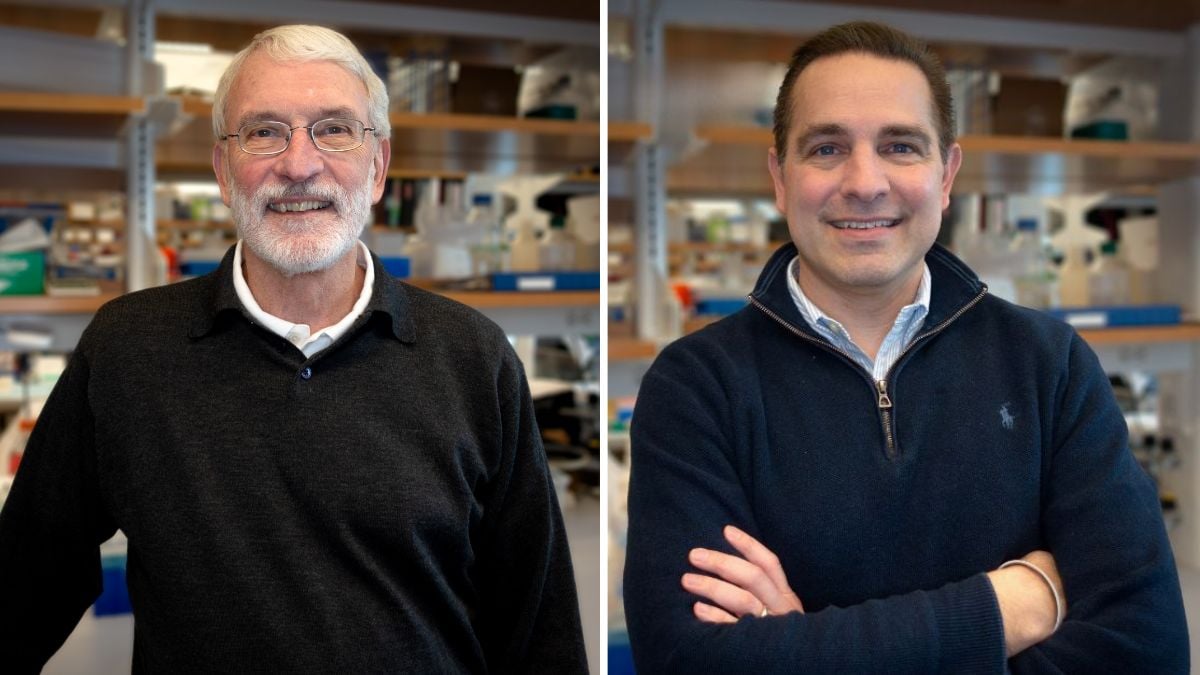
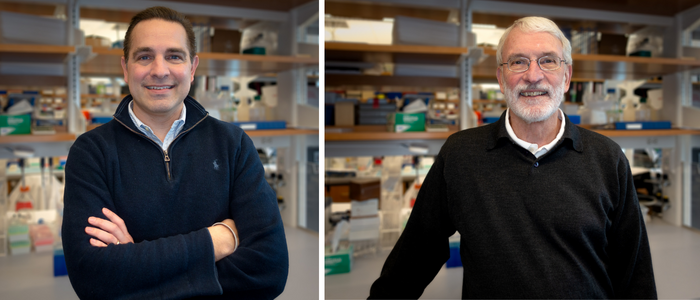
![Michael Brehm and Dale Greiner UMass Chan Diabetes Research]()
-
Friday, May 31, 2024
-
Tuesday, April 02, 2024
![Michael Brehm, PhD]()
-
Thursday, March 28, 2024
![Najihah Aziz Three Minute Thesis Winner]()
-
Friday, March 01, 2024
![Keri Walko-Henry, ATR, CCLS, LMHC]()
-
Wednesday, January 10, 2024
![Developing NAFLD Screening in the Clinic for People with Diabetes & Prediabetes]()