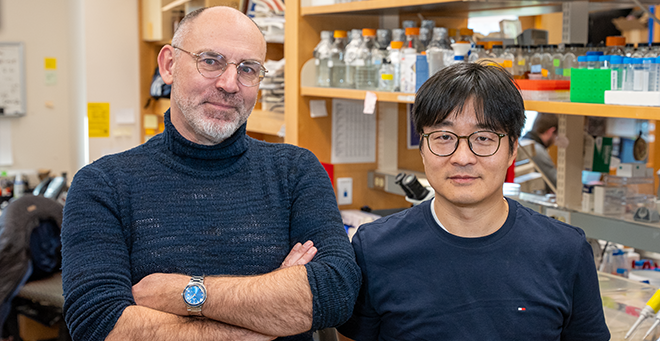
A new study published in Nature Cell Biology by Mark Alkema, PhD, professor of neurobiology, establishes an important molecular link between specific B12-producing bacteria in the gut of the roundworm C. elegans and the production of acetylcholine, a neurotransmitter important to memory and cognitive function.
There is growing recognition among scientists that diet and gut microbiota may play an important role in brain health. Changes in the composition of the microbiome have been linked to neurological disorders such as anxiety, depression, migraines and neurodegeneration. Yet, teasing out the cause and effect of individual bacteria or nutrients on brain function has been challenging.
“There are more bacteria in your intestine than you have cells in your body,” said Woo Kyu Kang, PhD, a postdoctoral fellow in the Alkema lab and first author of the current study. “The complexity of the brain, the hundreds of bacterial species that comprise the gut microbiome and the diversity of metabolites make it almost impossible to discern how bacteria impact brain function.”
To isolate the impact of individual bacteria on specific brain functions, Dr. Kang fed a diet made up of a single bacterial species to worms with a mutation that results in an imbalance in excitatory/inhibitory signaling in the brain and leads to seizure like-behaviors in the worm. A similar genetic mutation in humans causes migraines.
Kang fed these mutant C. elegans diets of a single bacterial species and watched for changes in seizure frequency. Out of the 40 different bacterium diets he tested, 18 reduced the number of seizures. Further experiments showed that the common attribute between a number of these bacteria was their ability to produce vitamin B12.
According to Dr. Alkema and Kang, B12 reduces the levels of choline in the body. Choline, a compound found in various foods and essential to metabolizing fat in the liver, can be used in the B12-dependent methionine/S-adenosyl methionine (Met/SAM) cycle, a metabolic pathway that produces methionine (an amino acid acquired by humans through diet that is essential to metabolism) in the intestine. However, choline is also used to make the neurotransmitter acetylcholine in the nervous system. Too much acetylcholine leads to the excitatory imbalance that causes the seizure-like behavior in the mutant worms.
When more B12 is present, more choline is used in the Met/SAM cycle, leaving less choline to produce acetylcholine. Reducing the amount of acetylcholine restores the excitatory/inhibitory balance in the nervous system and reduces seizure activity in C. elegans.
The researchers pointed out that the impact of “crosstalk” between the microbiome, vitamin B12, brain function and behavior only become apparent under conditions where the organism is stressed either genetically or environmentally. A deficiency of B12 in humans has been associated with neurological disorders that are characterized by excitatory/inhibitory imbalance such as schizophrenia, depression and migraine headaches.
“It will be interesting to determine whether the molecular mechanisms discovered in the worm can also explain the impact of B12 on excitatory signaling in several human neurological disorders,” said Alkema.
By using other worm models for other human diseases and testing other metabolites and bacteria, Alkema and colleagues hope to reveal other connections between the gut microbiome and brain function that can also be used to improve human health.
This study was funded in part by the Riccio Fund for Neuroscience and the National Institutes of Health and was a collaboration between the Alkema and Walhout labs at UMass Chan and the lab of Frank C. Shroeder, PhD, professor of chemistry & chemical biology at Cornell University.