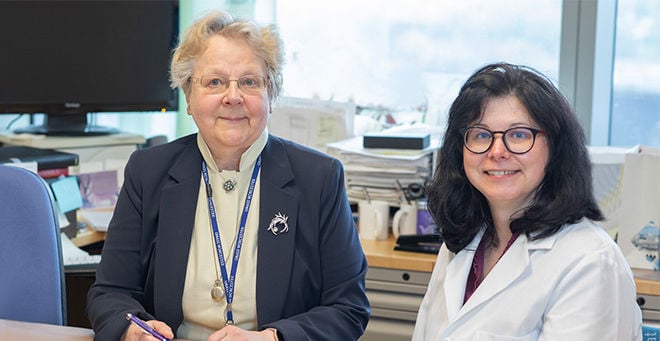
A study led by UMass Chan Medical School viral immunologists Liisa Selin, MD, PhD, and Anna Gil, PhD, discovered similarities in immune system dysfunction as a potential biomarker among people living with long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). The research also introduced a novel treatment and a method to track effective treatment interventions. The research was published online in Brain, Behavior & Immunity Health.
Dr. Selin, professor of pathology, and Dr. Gil, instructor in pathology, have been working to understand the connection between long COVID and ME/CFS and their overlapping symptoms, such as debilitating, unrelenting exhaustion and a worsening after physical or cognitive exertion, a symptom known as post-exertional malaise. In the new study, researchers identified a set of CD8 T cell cytokine biomarkers that distinguished the long COVID and ME/CFS patient groups from the control group. CD8 T cells are an important immune cell for fighting viral infections and cancer by making special cytokines. Depending on their type, composition and context, cytokines can either help or hinder the body’s immune and inflammatory responses to infectious diseases and other insults. According to the study, people with long COVID and ME/CFS had dysfunctional CD8 T cells, decreasing their ability to produce helpful cytokines. This dysfunction was associated with symptoms such as exhaustion and cognitive dysfunction.
Preliminary results from a small, retrospectively assessed group treated with the novel agent Inspiritol, showed an improvement in CD8 T cell function that paralleled patient reports of reduced symptoms, including fatigue and cognitive difficulties over the course of treatment.
“This work represents a great advancement in helping characterize long COVID and ME/CFS, and, potentially, to measure the effectiveness of promising treatments. Additional studies, including large and fast-tracked clinical trials of treatments, should be conducted to further validate our findings,” Selin said.
Read the entire research paper online in Brain, Behavior & Immunity Health.