 |
|
|
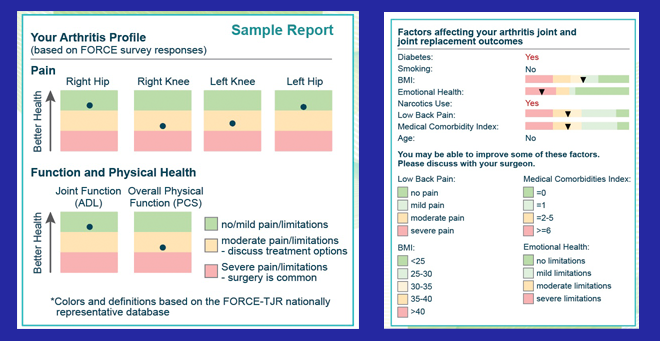
The web-based A.S.K. decision-making tool compares an individual’s information with nationwide population data to help patients and doctors decide if and when to proceed with total joint replacement surgery. |
A new web-based tool developed at UMass Medical School helps patients with osteoarthritis of the knee or hip decide if and when to proceed with total joint replacement surgery by comparing the individual’s pain and function with nationwide population data. The decision-support tool called A.S.K. (Arthritis care through Shared Knowledge) is now deployed in a two-phase randomized controlled clinical trial with 40 orthopedic surgeons and 8,000 patients nationwide.
“As the burden of knee and hip osteoarthritis increases among aging adults, more patients elect total joint replacement. However, no clear guidelines exist for patients to determine the need for or the timing of surgery,” said Patricia Franklin, MD, MBA, MPH, professor of orthopedics & physical rehabilitation. Dr. Franklin is principal investigator for the five-year, $6.4 million grant from the Patient-Centered Outcomes Research Institute that funded the tool’s development and ongoing testing and refinement.
“Our initial pilot group of patients of two surgeons who tested our novel web-based, patient assessment system appreciated the value of quantifying their severity of knee or hip pain, functional limitation, and individual goals for care for discussion about the risks and benefits of non-operative or operative care with their orthopedists,” she said.
The assessment was developed with findings from the UMMS-led Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement. FORCE-TJR is the most comprehensive U.S. database on total hip and knee joint replacement patients, and includes patient-reported outcomes as well as surgical and implant data. Surgeons and patients in Massachusetts, Connecticut, Pennsylvania and New York collaborated with the researchers to refine the content and presentation of the data to ensure ease of use and interpretation.
The patient assessment system presents individualized osteoarthritis care plan alternatives derived by analyzing patient-reported pain and symptoms; provides estimates of likely total joint replacement outcomes based on patient risk factors such as other medical conditions; and presents evidence-based information for non-operative as well as operative care. The information is personalized in the context of a patient’s goals for pain relief and improved function, and is available in real time for discussion during an orthopedic office visit.
The study will compare the osteoarthritis care decision process and quality, and quality of care as measured by pain relief and functional gain, between patients who use the A.S.K. system and controls who receive care as usual at 6 and 12 months after the decision.
“We hypothesize that A.S.K. users, as compared to those who receive usual care, will report greater decision quality for both operative or non-operative care, with less pain and greater function after treatment,” said Franklin.
The research team hopes that lessons learned from A.S.K.’s automated, patient-centric decision support system can ultimately be translated to phone-based apps to further engage and inform patients considering other elective surgical procedures.