Failure to Thrive
Objectives:
- Review normal growth parameters for infants and children
- Define failure to thrive (FTT) using objective growth parameters
- Remember that FTT is a symptom, not a diagnosis, with a long differential!
- Review common causes of FTT in children
- Discuss role of diagnostic evaluation, e.g. labs/imaging
Articles:
- UpToDate: Normal Growth Parameters in infants and pre-pubertal children
- Clinical Review of Failure to Thrive in Pediatric Patients, Larson-Nath and Biank, 2016.
- Failure to Thrive: A Consequence of Undernutrition, Gahagan, 2006 from Pediatrics in Review. Contains 2 imbedded cases.
- Failure to Thrive: Current Clinical Concepts, Jaffe, 2011 from Pediatrics in Review
Additional Resources:
- CHOP Clinical Pathways has one on Failure to Thrive, with futher articles referenced
- Peds RAP has 2 episodes on FTT, and part 1 is free!
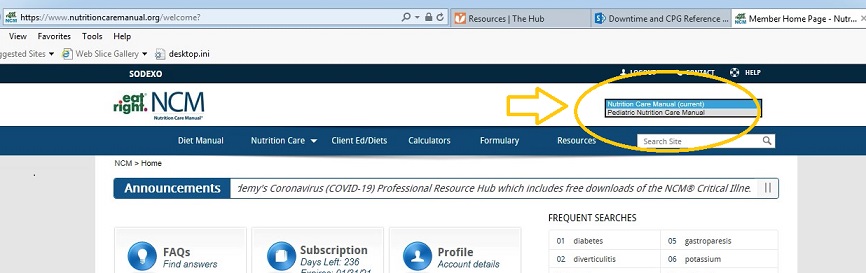
- See the Pediatric Nutrition Care Manual available on the Hub under Resources > Nutrition care manual > switch to Pediatric Nutrition Care manual
Self-Assessment:
1. A 1-month-old boy is referred to the emergency department from his pediatrician’s office because of failure to thrive. He was born at 36 weeks of gestation to a 20-year-old gravida 1, para 0 woman. She had appropriate prenatal care, and no complications were reported during the pregnancy or delivery. Perinatal testing results were unremarkable. The neonate’s birthweight was 2.5 kg. He breastfed well in the nursery, passed meconium and urine within the first 24 hours, and was discharged from the hospital on day 2 after birth. His discharge weight was 2.32 kg. By his first health supervision visit, at age 10 days, he had regained his birthweight. Since then, the boy has had progressively increasing problems with feeding. He typically feeds for 10 minutes on each side, with a burping in between, and seems to adequately empty both breasts. For the last several days, he has had increasing vomiting with each burp, as well as after the feedings. The emesis is the color of milk, sometimes digested, and not projectile. It is more than would fill a teaspoon. The last 2 days before presentation, he has not been interested in feeding.
His current weight is 2.41 kg. His temperature is 37°C, heart rate is 120 beats/min, respiratory rate is 24 breaths/min, and blood pressure is 70/40 mm Hg. Physical examination reveals a poorly nourished infant who is sleeping comfortably. He is easily aroused, remains calm, and quickly falls back to sleep. Mucous membranes are dry, and his sclera are slightly icteric. He has skin tenting and muscle wasting. The infant is breathing comfortably, lungs are clear, and his heart has a regular rate and rhythm, with a soft, grade II/VI systolic crescendo-decrescendo murmur heard best in the right upper sternal border. His abdomen is scaphoid, soft, nontender, and nondistended, with no palpable masses. He has normal male genitalia. Laboratory results are as follows.
- Laboratory Test Result
- Sodium 116 mEq/dL (116 mmol/L)
- Potassium 3.0 mEq/dL (3.0 mmol/L)
- Chloride 68 mEq/dL (68 mmol/L)
- Bicarbonate 40 mEq/dL (40 mmol/L)
- Glucose 62 mg/dL (3.4 mmol/L)
Of the following, the diagnostic test MOST likely to reveal the underlying cause of the infant’s electrolyte disturbance is
- Abdominal ultrasonography
- Urine pH measurement
- Upper gastrointestinal radiography
- Plasma aldosterone/renin activity
2. 3-month-old female infant is brought to the clinic for difficulty with feeding and poor weight gain. She was born at 39 weeks’ gestation with weight at the 50th percentile and had no complications. The mother states that the infant has been waking to feed about 2 oz every 3 hours. She often takes up to 40 minutes to feed, gets sweaty during her feeds, and seems tired afterwards. Her weight is 4.6 kg (second percentile), and she is thin. She has crackles in the lower lung fields and a grade 3/6 systolic murmur heard best at the left lower sternal border. The liver is palpable 2 cm below the right costal margin. Echocardiography findings are significant for a ventricular septal defect. A nasogastric tube is placed and bottle/gavage feeds are initiated with standard formula while awaiting a return call from the cardiologist.
Of the following, the BEST feeding plan for this infant is
- 2 oz every 3 hours
- 3 oz every 3 hours
- 4 oz every 3 hours
- 5 oz every 3 hours
3. A 12 year old boy is brought to your office for a health supervision visit. His body mass index has dropped from 50th to the 20th His mother reports that he has developed anxiety around eating and is not eating as much as he used to following an episode of food impaction several months ago. He was able to clear the impaction prior to evaluation in the emergency department. He reports no dysphagia, odynophagia or emesis. He now takes longer than the entire family to eat and is drinking large volumes of water with meals. His medical history is positive for eczema and asthma.
He has normal vital signs. He appears to be thin and is in no distress. He has no oral lesions. His abdomen is soft, nontender to palpation and without mass. Of the following the most likely diagnosis is:
- Achalasia
- Eosinophilic esophagitis
- esophageal stricture
- gastroesophageal reflux disease
- nutcracker esophagus
4. A 14-year-old adolescent is brought to your office for fatigue and decreased appetite that she has experienced over the past month. She has associated nausea but no vomiting, diarrhea, or fever. Her medical history is significant for autoimmune hypothyroidism since age 8 years, for which she takes levothyroxine daily. Physical examination reveals a temperature of 37°C, heart rate of 120 beats/min, blood pressure of 90/48 mm Hg, respiratory rate of 16 breaths/min, weight of 44.6 kg (25th percentile), height of 165 cm (75th percentile), and body mass index of 16.4 kg/m2 (10th percentile). She appears tired, with diffusely hyperpigmented skin. Capillary refill time is 3 seconds. The remainder of her physical examination findings are unremarkable.
Of the following, this girl’s MOST likely diagnosis is
- adrenal insufficiency
- anemia
- anorexia nervosa
- gastroparesis
- uncontrolled hypothyroidism
5. A 6-year-old boy with autism has been hospitalized for apparent leg pain, weakness, and refusal to walk. His diet consists exclusively of “white foods,” notably mashed potatoes, chicken nuggets, and plain macaroni. Water is his only beverage.
His physical examination shows an afebrile nonverbal child with diffuse extremity tenderness, without swelling or deformity. He has inflamed gums with mild bleeding, several bruises on his legs, and a hemorrhagic follicular rash on his buttocks. The remainder of his examination findings are within normal parameters. Laboratory findings include normal prothrombin and partial thromboplastin times; a mild microcytic anemia but an otherwise normal complete blood count; normal liver and renal functions; and normal alkaline phosphatase, calcium, and phosphorus levels. Radiography shows osteopenia and a distal femur metaphyseal fracture.
Of the following, the laboratory test MOST likely to help determine the cause of this child’s symptoms is
- 1,25 dihydroxy-vitamin D level
- antinuclear antibody and rheumatoid factor
- creatine kinase level
- leukocyte ascorbic acid concentration
- nasopharyngeal viral cultures
6. You are seeing a 4-month-old infant with poor growth and an enlarged abdomen for follow-up care after an emergency department visit. The parents state that they have taken the infant to the emergency department on several occasions for low blood sugar after the baby began to sleep through the night. One of these episodes was associated with a seizure.
The infant has doll-like facies with fat cheeks, protuberant abdomen, hepatomegaly, renomegaly, short stature, and thin arms and legs. No splenomegaly is noted.
You order laboratory tests that reveal elevated lactate, uric acid, and lipid levels, along with a low serum glucose level. Liver transaminases, complete blood cell count, and hemoglobin A1C are within the normal range. You order an echocardiogram that rules out a congenital heart defect with associated congestive heart failure.
The family history is unremarkable, and the infant’s developmental milestones are appropriate.
Of the following, the MOST likely disorder to present with these clinical and laboratory findings is
- Gaucher disease
- glycogen storage disease type I
- Hurler syndrome
- peroxisomal disorder
- Pompe disease