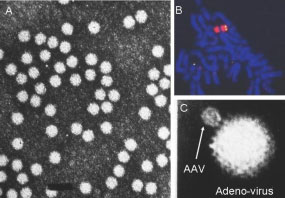
Adeno-associated virus vectors (AAV)
AAV is a non-pathogenic human parvovirus which is commonly isolated from the respiratory tract of humans (Figure 1A). AAV’s life cycle includes a unique mechanism for persistence in human cells by means of site-specific integration into a region of chromosome 19, the AAVS1 site (Figure 1B).
 In 1993, our group published the results of the first successful in vivo gene transfer with AAV. In that study, AAV vectors carrying the human CF transmembrane conductance regulator (CFTR) gene were delivered to the bronchial epithelium of rabbits. Efficient gene transfer was observed which persisted for over 6 months without any detectable toxicity. Subsequently, we studied AAV-CFTR gene transfer in rhesus macaques. Our studies in rhesus served two purposes: 1.We performed the primary toxicology study to justify beginning our phase I trial of AAV-CFTR administration in humans, and 2. we studied vector integration and persistence in vivo for the first time.
In 1993, our group published the results of the first successful in vivo gene transfer with AAV. In that study, AAV vectors carrying the human CF transmembrane conductance regulator (CFTR) gene were delivered to the bronchial epithelium of rabbits. Efficient gene transfer was observed which persisted for over 6 months without any detectable toxicity. Subsequently, we studied AAV-CFTR gene transfer in rhesus macaques. Our studies in rhesus served two purposes: 1.We performed the primary toxicology study to justify beginning our phase I trial of AAV-CFTR administration in humans, and 2. we studied vector integration and persistence in vivo for the first time.
Since then our laboratory has gone on to perform phase I clinical trials delivering AAV2 expressing the CFTR gene in CF patients. Much has been learned form the early trials including that paucity of AAV2 receptors on the luminal side of the airways and the weak promoter activity in early vectors.
This limited the efficiency and efficacy of the viral vectors used in the early trials. To overcome this, the lab has designed a more robust expression cassette delivering a CFTR ‘mini’ gene and has determined that AAV1 is far superior to AAV2 at transducing airways. These new generation viral vectors for CF gene therapy are currently undergoing pre-clinical testing and will soon be tested in patients. Our laboratory has also pioneered phase I clinical studies using intra-muscular administration of rAAV2 as well as this more novel AAV1 serotype expressing the gene for alpha-1-antitrypsin (AAT) in AAT deficient patients.
We are also developing hybrid rAAV-RNAi approaches to treat AAT deficient liver disease in which a toxic gain of function of the mutant protein contributes to the pathology. The laboratory is also involved in gene therapy for fatty oxidation disorders. Specifically we are developing gene delivery for the Acyl-CoA Dehydrogenases family enzymes that initiate the first step of the B-oxidation pathway.