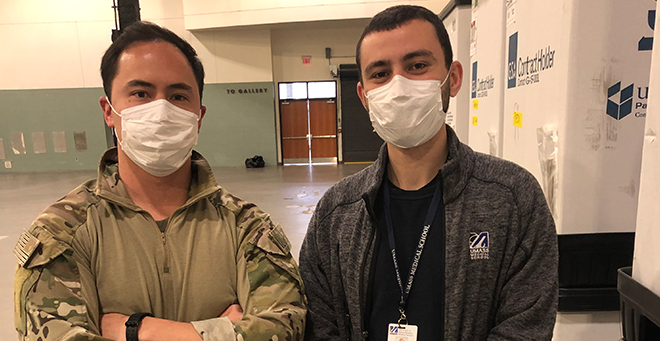
Blake Foster, SOM '21 |
A School of Medicine student and a recent graduate are helping the region prepare for a potential surge of COVID-19 patients by readying the city’s DCU Center to function as a field hospital.
The unit, in the center’s main exhibition hall, is designed to hold up to 250 patients with milder cases of the novel coronavirus infection. It will be licensed by the state and operated by UMass Memorial Medical Center.
Grant Lewandrowski, MD, received his medical degree on March 31, two months ahead of the originally scheduled ceremony, and is slated to begin a residency in family medicine at UMass Memorial in July. His self-designed, fourth-year elective program combining emergency medical services, disaster medicine and tactical medicine, as well as a background in the U.S. Marines Corps, led him to put his training into action now to combat the pandemic.
Blake Foster will complete a fifth year in the School of Medicine, conducting research as he applies for a residency in emergency medicine, after changing his future specialty from anesthesiology. He brings his own experience with wilderness survival skills, along with his medical training, to help engineer the DCU field hospital.
Since the pandemic exploded locally over the past month, “It’s been all hands on deck,” Dr. Lewandrowski said.
“We’ve had the same training,” he said, citing collaboration across specialties to provide COVID-19 services. “Whether we’ve been trained in one bone or one cell, we’re all physicians at heart.”
Leading up to the DCU field hospital project, the duo built out the interior of the COVID-19 screening tent outside UMass Memorial’s emergency bay, in March. A tent shell existed, but workflow areas needed to be set up to accommodate sick patients coming in and keep them separate from uninfected patients and staff.
Lewandrowski was working on his elective with John Broach, MD, MPH, assistant professor of emergency medicine and director of the Division of Disaster and Emergency Preparedness, and and Matthew Rebesco, MD, assistant professor of emergency medicine. They had purchased rope, duct tape, zip-ties and shower curtains, with which they tried to jury-rig a makeshift medical ward.
“We needed an expert at tying knots,” Lewandrowski said. So he called Foster, an experienced outdoorsman, and they “cranked out the entire interior in a day and a half.”
“Grant and I share a passion for disaster medicine,” Foster said. “With his military background and my wilderness experience, we make a really good team.”
The DCU field hospital is on a much larger scale, with equipment shipped in from the Federal Emergency Management Agency and National Guard troops helping with the buildout.
It’s not clear yet how many patients will need the surge space, which is intended to allow area hospitals to devote their resources to treating the sickest patients. It is targeted to open around April 9, Foster said.
“While it’s not needed immediately, it’s better to have in place while we have the leeway and breathing space to do it right, rather than under duress with 300 patients needing it,” Foster said.