|
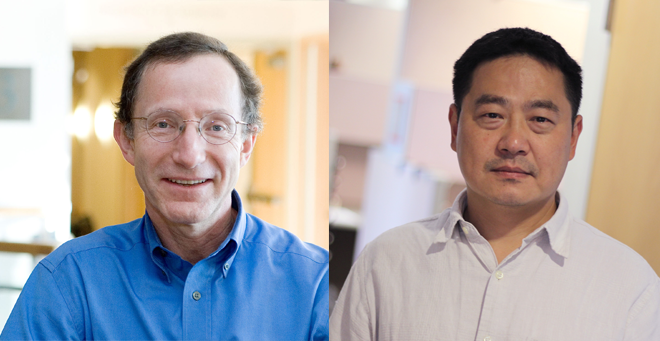
Hardy Kornfeld, MD, is co-principal investigator of a clinical trial to help improve tuberculosis treatment. Funded by a five-year, $2.9 million grant from the National Institutes of Health, the trial will help determine whether adding the widely available and inexpensive diabetes drug metformin to standard antibiotic treatment can yield better outcomes for nondiabetic patients with tuberculosis and human immunodeficiency virus (HIV).
“Evidence suggests that patients with diabetes who are treated with metformin have a lower risk of progressing to active tuberculosis, a lower risk of failing treatment and a lower risk of tuberculosis relapse,” said Dr. Kornfeld, professor of medicine in the Division of Infectious Disease. “Metformin can be given safely to people who do not have diabetes, because it works by a mechanism that doesn’t reduce blood sugar levels.”
TB is well controlled in the United States, but remains a leading cause of death and disability worldwide. Many of those with TB don’t finish the treatment necessary to achieve a cure; with or without antibiotic treatment, the illness still causes irreversible lung damage in half of survivors. When tuberculosis is present along with HIV, the virus that causes AIDS, the prognosis for surviving both diseases is worse.
Enter metformin, which may be effective as what is known as a host-directed therapy (HDT) to enhance standard antibiotic therapy. Unlike antibiotics, HDT drugs act by directly modulating host cell functions, fine tuning the antimicrobial activities of host immune cells and limiting the lung inflammation and tissue damage associated with tuberculosis.
“We hope that HDT shortens the duration of treatment necessary to achieve cure and preserves lung function by controlling inflammation,” said Kornfeld. “In this study, we focus on TB/HIV co-infection because these individuals have the greatest need for better tuberculosis therapies; because metformin specifically boosts the component of cell-mediated immunity that is preserved in HIV; and because metformin is predicted to exert host-directed therapeutic activity against HIV as well as TB.”
HIV/TB patients tend to be sicker and thus may have greater potential to benefit from enhanced treatment. The need for better TB treatment is most acute in South Africa, which is home to 0.7 percent of the world’s population but has 17 percent of the global burden of HIV infection and one of the world’s highest incidences of tuberculosis. The study team at the Aurum Institute in Tembisa, South Africa, will recruit 112 subjects infected with TB and HIV to participate in the trial.
Wenjun Li, PhD, associate professor of medicine and chief statistician for the trial, will analyze the data. “This study turns talk into action with the first human trial: two treatments, one for TB, one for HIV, in conjunction with metformin, creates opportunities to study their interactions,” said Dr. Li. “We can then design larger trials to find out which treatments provide the most benefit for which group of patients, so future treatment can be targeted.”
“We predict that metformin will speed up the response to antibiotics and prevent lung damage that afflicts half of all patients who are cured of tuberculosis,” said Kornfeld. “Positive results from this clinical trial could change the way that tuberculosis is treated around the world.”