 What are the best treatments for vitiligo? Many times patients go to their doctor and they’re told, “There’s no cure for vitiligo”. Well that's true, but that doesn’t mean there aren’t good treatments! Also, we talk a lot on here about our excitement for new treatments for vitiligo, and sometimes that sounds like “current treatments don’t work”. Well, that’s NOT true. We have good treatments, but we’re trying to make better ones.
What are the best treatments for vitiligo? Many times patients go to their doctor and they’re told, “There’s no cure for vitiligo”. Well that's true, but that doesn’t mean there aren’t good treatments! Also, we talk a lot on here about our excitement for new treatments for vitiligo, and sometimes that sounds like “current treatments don’t work”. Well, that’s NOT true. We have good treatments, but we’re trying to make better ones.
So what are the best treatments for vitiligo? The answer is pretty simple. Get out your pen, and I’ll tell you exactly what I do when patients come to my clinic. It’s not a secret!
When I see vitiligo patients I ask the typical questions, like when it started, where it started, whether it’s active or stable, and what they have tried so far. I ask whether anyone in their family has vitiligo or other autoimmune diseases, and then ask a few questions to determine whether they might have additional autoimmune diseases that they don’t know about. I ask about exposure to vitiligo-inducing chemicals, which you can read about here. I then look at their skin and all their spots to determine how much of their body is affected by vitiligo, and whether there are any signs that it’s active, highly active, stable, or getting better. I usually use a Woods lamp (also called a “black light”) to help me see any changes that might not be visible by room light, and I may take out a special magnifying glass to help me see the spots up close. I try to determine if the spots could be from something other than vitiligo, which I see frequently, and need to treat differently. I don't usually need to do a skin biopsy or blood tests, but occasionally do them when the clinical picture isn’t clear.
Based on what I see, hear, and sometimes feel, I work with the patient to develop a treatment plan. It’s not the same for everybody, because the disease extent, activity, and location for each patient is different. They also have different insurance plans, different resources, live in different places, and have different emotional reactions to their vitiligo. For example, some patients choose to continue using hair dyes even though they could be making their disease worse, and others stop them immediately. Either choice is ok, because the patient has the final say.
If the patient just has a few spots, then we use a potent topical steroid twice daily for a week, alternating with tacrolimus twice daily for the next week to start. For kids I usually use a less potent steroid since they’re still growing and their skin is a little more delicate. They keep using this back and forth until I see them again in a couple months. I tell them that they shouldn’t expect to see results for 2-3 months. If the spots are on the face, genitals, breasts, or underarms, I tell them to only use tacrolimus, since these areas are more sensitive to chronic steroid use. If they’ve already tried these without a good enough response, I’ll suggest excimer laser treatment, which is very effective for small areas. The face is very responsive to all of these treatments, and patients are usually happy with them.
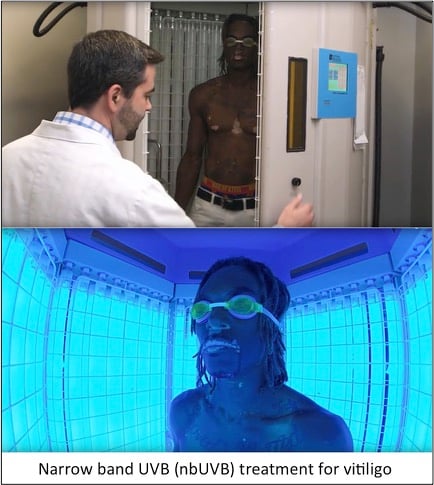
If the patient has too many spots for just topical treatments (usually more than 5% of their body surface covered), I strongly recommend they use narrow band UVB (nbUVB) phototherapy, which is offered at many dermatologists’ offices around the country. For those who have traveled to our clinic from a distance and therefore can’t get their treatment directly from us, we try to help them find a location that offers it closer to their home, and we’re often successful! This treatment requires 2-3 visits per week, each treatment takes only 1-4 minutes, and again it takes 2-3 months to start seeing the improvement. However the way that nbUVB treatment is given is very important – if not done correctly it may not work well, if at all. That’s why I prefer to treat patients myself in our booths, but if they live too far away, I give them a copy of our protocol for the therapy to give to their doctor in case he or she is willing to use it – it can be found here. Sometimes patients opt for purchasing a nbUVB unit for their home, and we help them do this. Many times insurance doesn’t cover it though, and they have to pay for it themselves. I also suggest patients use topicals on areas that are highly visible or otherwise important to them in addition to phototherapy.
If patients have rapidly expanding disease, such that they’re getting new spots every week and the existing ones are getting bigger, we talk about starting oral steroids, which help to slow the spread of disease. Sometimes I give low dose steroids every other day, or only on Saturday and Sunday. We’ll continue this until the disease has stabilized and another treatment has started working for them. For patients with a lot of disease (more than 80% or so of their body covered), I will discuss Benoquin or monobenzone treatment, which “bleaches” or removes the rest of their color so that they look even, without spots. This isn’t for everybody, since it’s permanent and may decrease their chances of responding to the new treatments we keep talking about, so it’s a big decision that shouldn’t be taken lightly. For a very small number of patients, we discuss taking new treatments like JAK inhibitors, but usually patients have to pay the high costs of these medicines themselves. I have also had one or two patients travel to the Dead Sea to get intensive sun therapy for a few weeks, and they have had good responses.
After this discussion about treatments, I usually answer a bunch of questions, since that’s one of the reasons people come to see me in clinic, often from far away. While this can be challenging during a busy clinic, I always try to spend as much time as I can because I like it, and it’s important. This is why I frequently run behind, and patients end up waiting a while to see me. It stresses me out a bit, but I don’t know any other way to take care of my patients, and they’re usually pretty understanding. So as you can see, everyone needs a personalized approach, but the basic tools and principles are pretty simple.